The documentation review this month is slightly different than previous months, because the patient was not discharged prior to the bad outcome. The bad outcome was apparent prior to her departure from the ED. Also, the physician who was sued never wrote a note about the patient (nor should he have written a note).
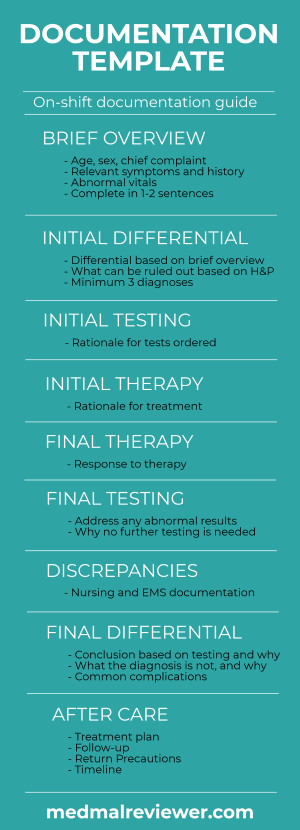
I will use the Documentation Rubric to guide the assessment of the physician’s note. If you want help writing notes in real-time, during your next shift, the Documentation Template is what you want. It will help improve your notes and make a positive outcome more likely.
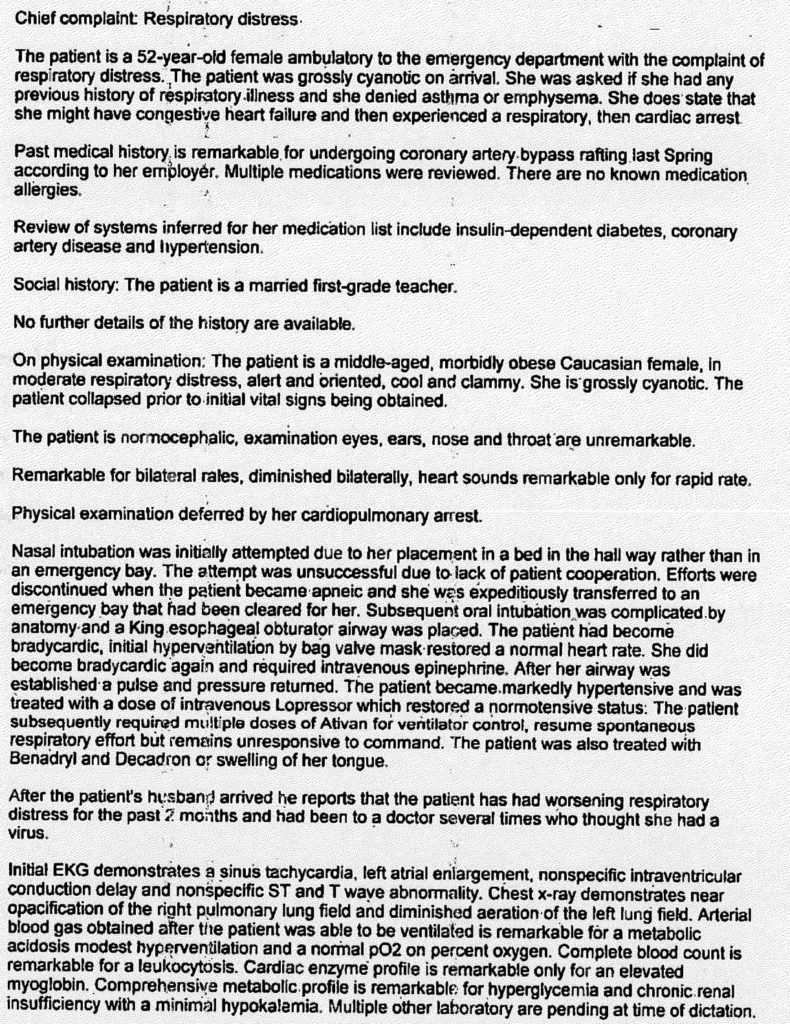
The note is shown again below for easy reference.
This case received a final score of 15/20.
Brief Overview: 2/2
There is a good brief overview of the patient’s condition listed under the physical exam. It describes the patient’s condition in 1-2 sentences and effectively communicates the relevant history and presentation. Ideally this would be found at the beginning of the MDM section.
Testing: 3/3
In the final paragraph of the physician’s dictation, he goes through the tests that were ordered and the relevant results. Too often, doctors merely copy/paste lab values and radiology interpretations into their note. This is useless repetition and clutters the documentation. The goal should be to demonstrate your interpretation of the results. He comments only on the relevant findings and what he considers to be useful information.
Therapy: 2/3
The medications that were ordered are clearly explained. The focus on addressing the patient’s hypertension is somewhat of an odd medical decision, but the reason and rationale for this decision is clearly explained by the doctor. He explains why Benadryl and Decadron were given. The reader is not left guessing why he gave a particular medication. However, we are left guessing why he didn’t give certain medications, including paralytic. It would have been useful to briefly address why he deviated from normal medication use patterns. Mentioning that no paralytics were used due to hospital policy would have been ideal.
Differential: 4/8
There is no explicit discussion of the potential causes of this patient’s worsening respiratory status leading to a respiratory arrest. The differential is long and could including MI/ACS, PE, fluid overload/CHF, flash pulmonary edema, pneumonia, among many other possibilities. Explicitly listing the differential is helpful because it makes the writer mentally consider the potential causes, which can help the doctor guide themselves through various testing and treatment options. We can deduce from the tests that were ordered that he had a differential in mind, but explicitly listing this differential would have been preferred.
Discrepanices: No deduction
Aftercare: 4/4
The aftercare in this case is not focused on discharge instructions, it is focused on arranging transfer to another facility. This is the topic that actually generated the lawsuit. The fact that the physician thoroughly documented his phone calls, who he spoke with, and what time, may have been key in avoiding being named in the lawsuit. It paints a clear picture of his actions and efforts in order to find a higher level of care for his patient.
I find it interesting that no mention of responsibility is made of the helicopter inter-facility transfer crew. While EMTALA certainly places the main responsibility for selecting the correct transport modality on the sending physician – there is some shared responsibility to manage the in-transport hypoxia – why was a new airway not placed, why was a crich not performed, etc… Those are well within the scope of any HEMS system in the US for the past >15 years. The helicopter is not just a vehicle – there is management that is required or else we should go back to the helicopter model from the Korean War (like in MASH).
Yes, it is very surprising that there isn’t much info about transport phase, where the critical transition from a salvageable to an almost dead patient happened. I wonder if there’s a separate lawsuit against chopper folks.
So they’ve got a chopper pad, but no sux, huh?
If a medical facility is unable to provide myorelaxation, should it be allowed to admit EM patients? They might as well have just called 911 and paramedics would do the job – a proper tube, crich or dil trach, then gave a ride to the appropriate facility.
Why any of that haven’t been done by the helicopter crew?
Why to discuss a transfer with a cardiologist? Isn’t it a ED to ED or ED to ICU exchange? How a consultant specialist ended up picking ED phone calls?
Looks like in this case it’s more about organizational defects and miscommunication than actual medmal.