Welcome to medmalreviewer.com! The purpose of this site is to improve doctor’s medical knowledge and documentation by reviewing real-life malpractice cases. The first case is below. These cases are presented in long form, deep dive fashion, and I’ll try to post one each month. Each case is broken down into 5 posts. To see more info about the website, here are links to the About Page and FAQs. Another helpful overview post is the 3 Goals of Documentation. I’ve created a Documentation Template to help doctors write notes that are easy to defend, and a Documentation Rubric to grade notes from malpractice cases.
Home Page
Post 1: Introduction
Post 2: Bad Outcome
Post 3: Legal Outcome
Post 4: Documentation Review
Post 5: Medical Review
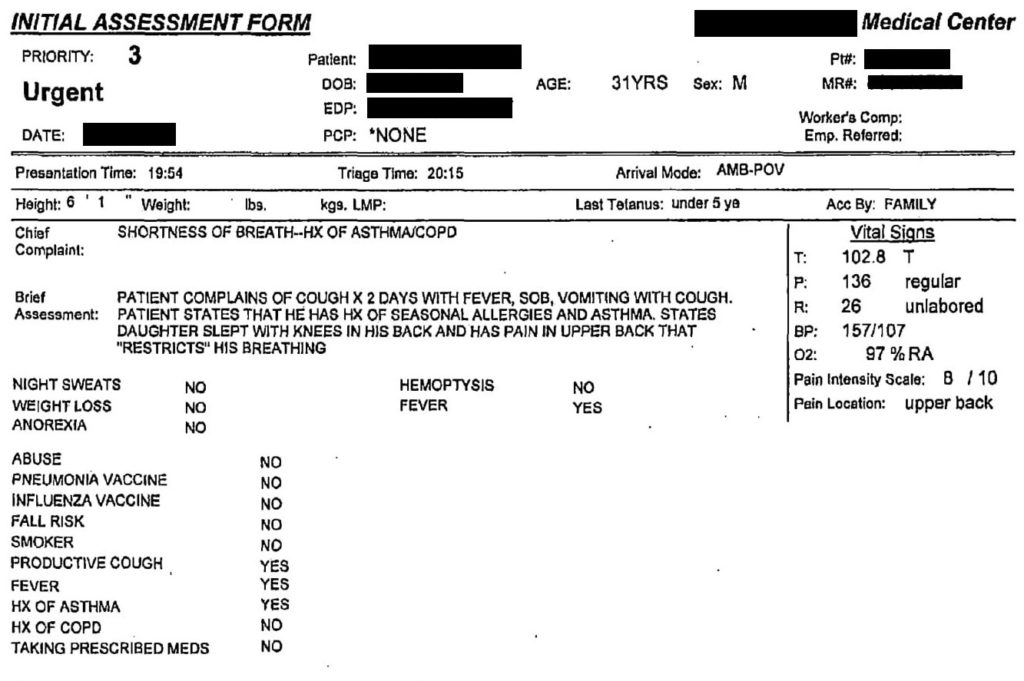
This case concerns a 31-year-old man, who presents to the ED with a chief complaint of shortness of breath. He checked into the ED at 7:54pm, and the triage note is shown below. The nurse has documented a cough for two days, fever, SOB, pain in his upper back that restricts his breathing, and a history of asthma. Vitals show that he is tachycardic, tachypneic and febrile but has a normal oxygen saturation and is slightly hypertensive.
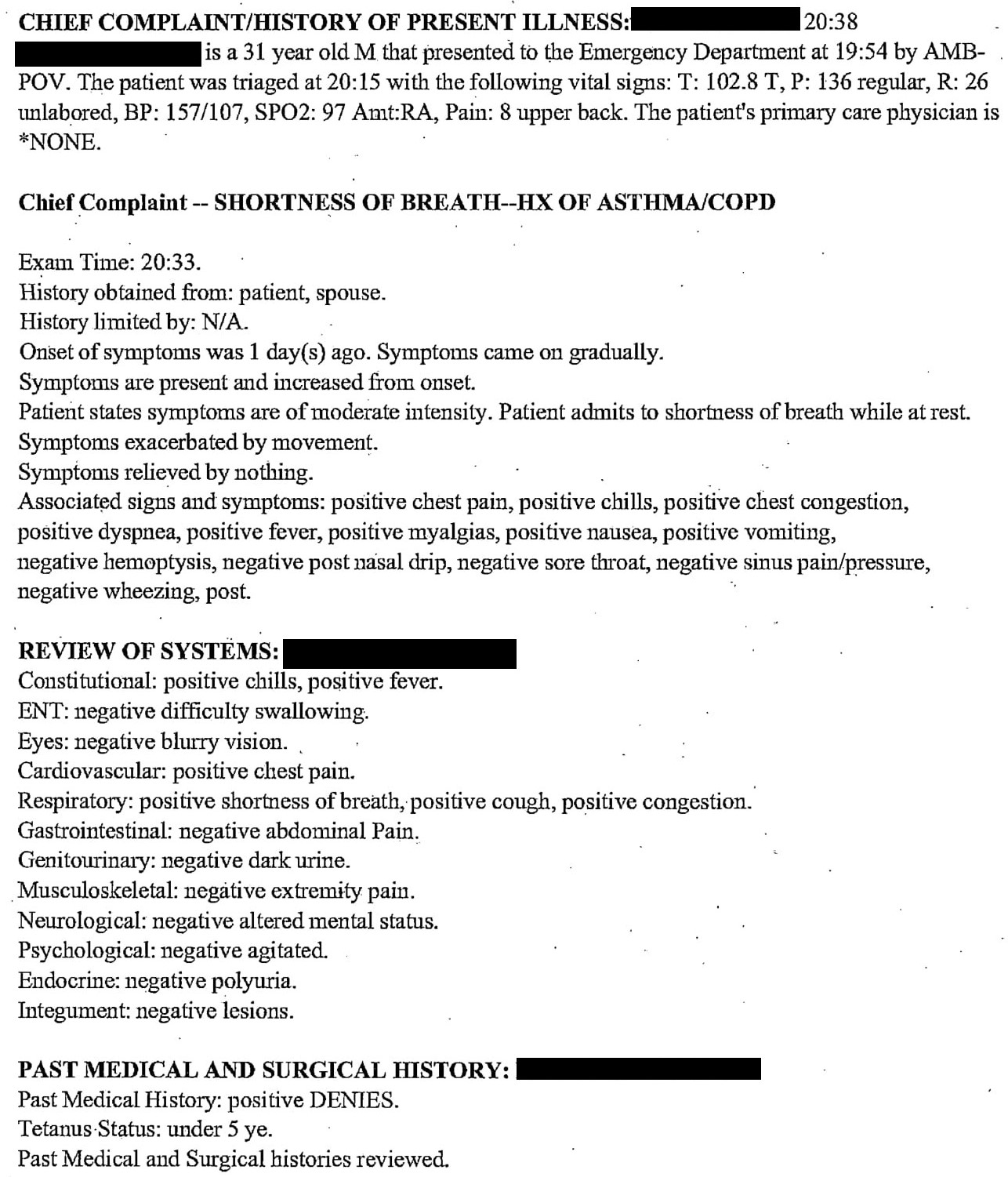
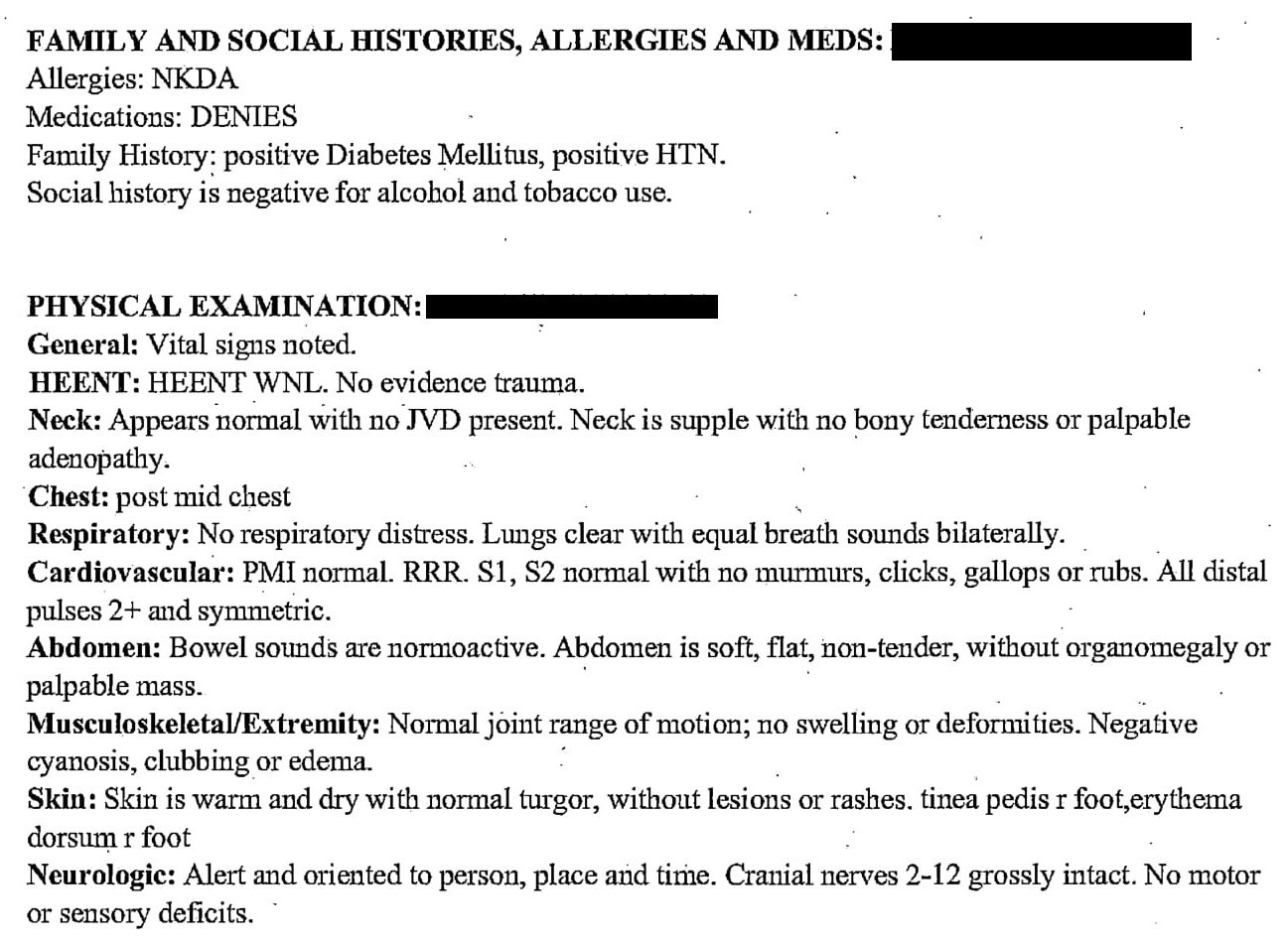
By 8:30pm, the ER doctor has seen the patient. The information from the physician’s note is largely the same as the triage note. Additionally, the symptoms are described as having been present for about 1 day, and have gradually worsened. He is short of breath at rest and has not found anything to relieve his symptoms. The doctor also notes chest pain and chest congestion.
At this point in the case, let’s pause and think. Any good ER doctor at this point will think about a differential, and then consider what tests need to be done to assess for the items on the differential. What would you think about and what tests would you order?
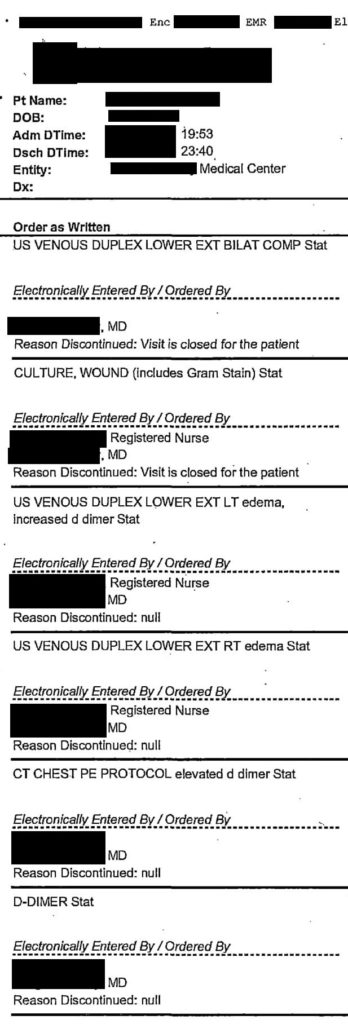
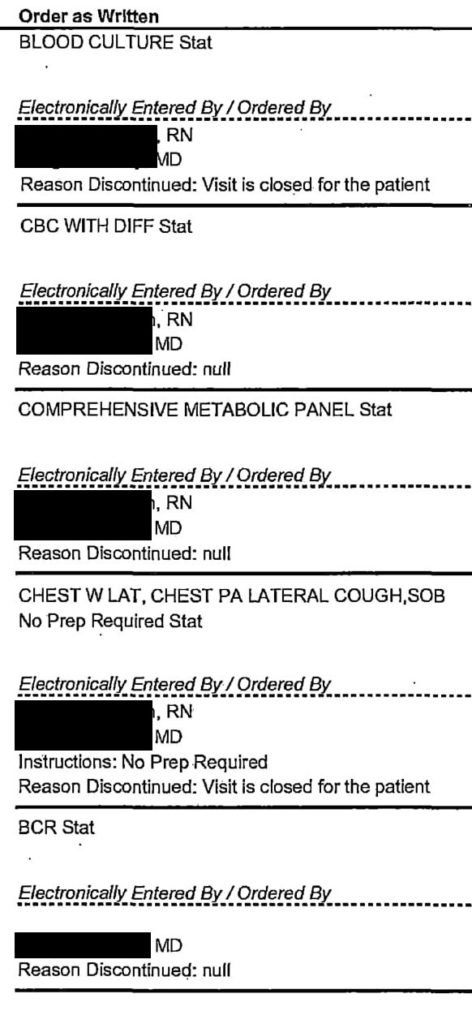
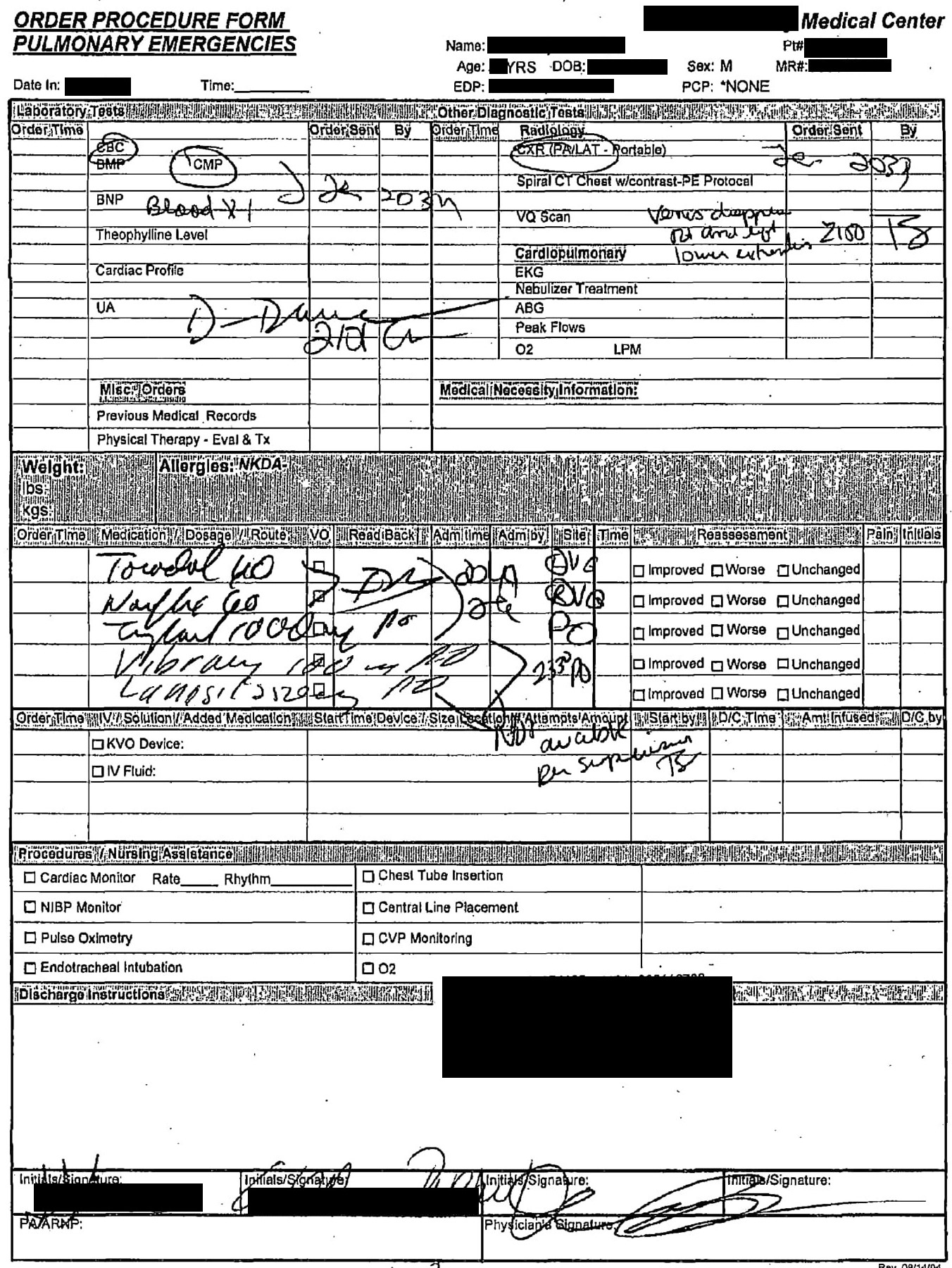
Unfortunately there’s nothing in the doctor’s note to indicate what he was thinking in regards to a differential. We do, however, have evidence of the orders that were placed. The orders were written by hand but are difficult to read, so we’ll review the version that was entered into the computer. The orders are: CBC, CMP, D-dimer, blood cultures, chest xray, bilateral lower extremity venous duplex ultrasounds, CT chest PE protocol.
In regards to medications, the patient was given Toradol 60mg, Norflex 60mg, Tylenol 1000mg, doxycycline 100mg and Lamisil 250mg.
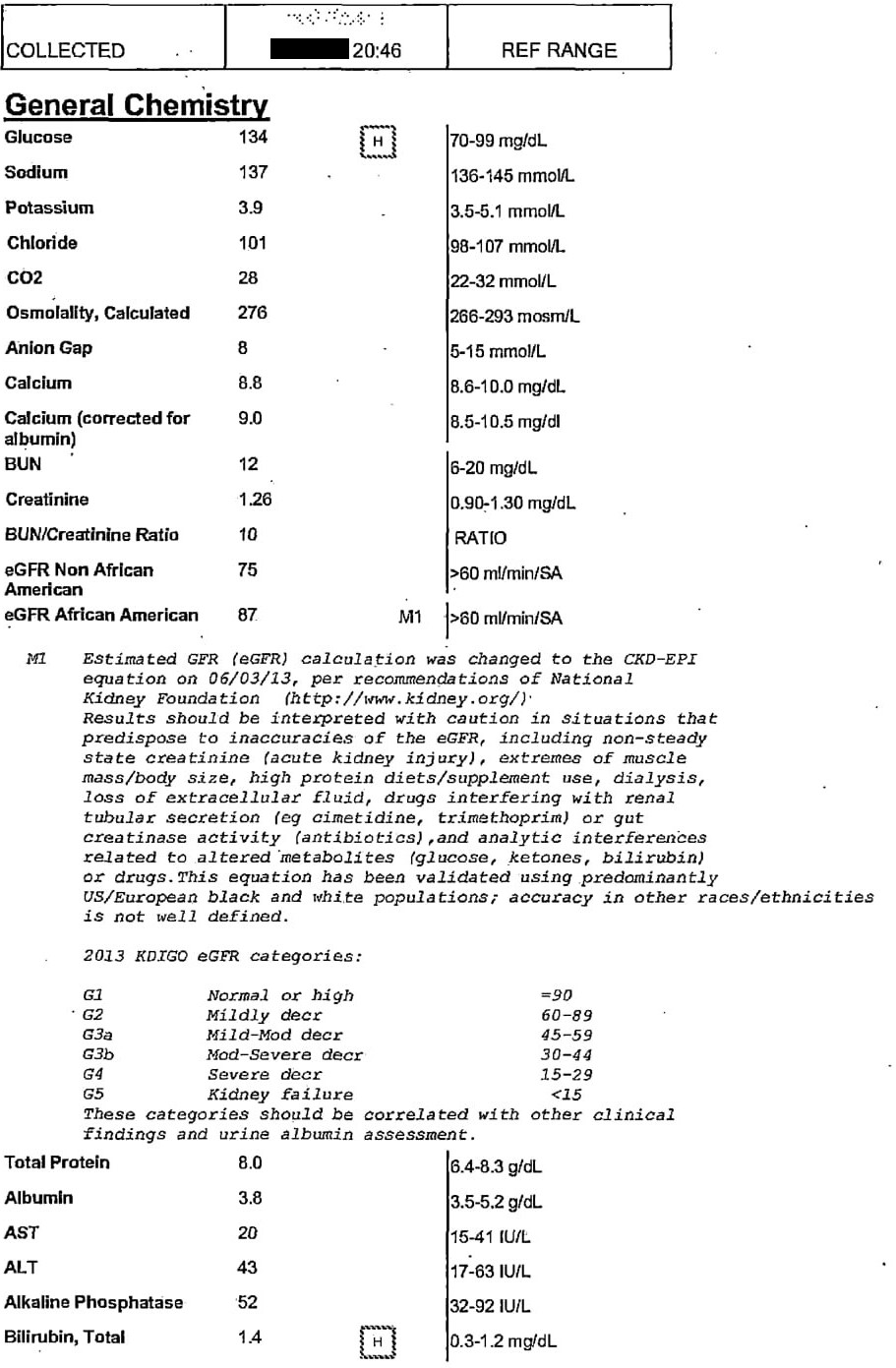
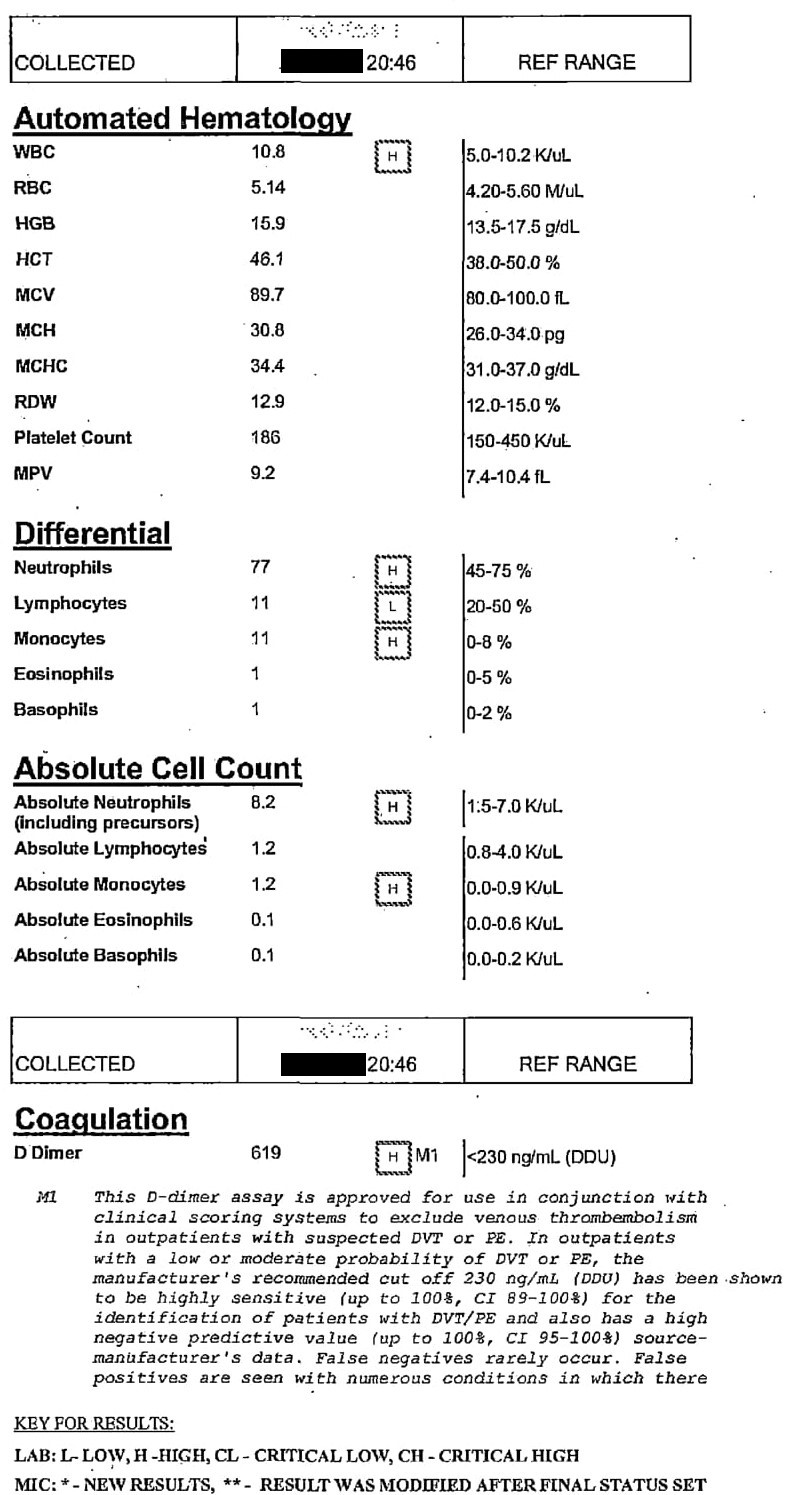
The lab results show elevated D-dimer. There are several other minor abnormalities as well. Obviously, blood culture results will not be back for some time and were not available to the clinician.
Imaging results are obtained. The ultrasounds of his bilateral legs do not show any sign of DVT.

The xray of the chest is unremarkable.
At this point it was discovered that the patient was too large for the CT scanner. He had a BMI > 50, and it was felt that the equipment would not be able to safely handle his weight. The remainder of the physician’s note is shown below. There is no discussion of the fact that the CT scanner was too big, nor the subsequent conversation that he had with the patient. Later depositions would suggest that the doctor told the patient that if his symptoms did not improve after a few days, that he should go to another hospital in order to have the CT scan.
The patient was given wound care to the erythematous right foot/5th toe.
He was then discharged from the ED around 11:30pm with a diagnosis of acute bronchitis and cellulitis/tinea pedis. He was instructed to continue taking doxycycline, Lamisil, and Zanaflex.
The nurse taking care of this patient documented a thorough note, including the discharge vitals. Click here to read the nurse’s note.
How would you have managed the situation differently?
What do you think happens next?
What will the outcome be?

PE had to be ruled out. He gets full anticoagulation until a study demonstrates otherwise.
I think you are obligated to get a CT scan or V/Q scan some how. If that means admitting the patient putting them on heparin (lovenox hard to dose in obese patients) and let the admit team deal with the transfer.
Or if you documented a discussion with the patient regarding needing to get a CT scan — then that would be reasonable.
But look, lets be honest here. The patient is fat. And the doctor’s plan was to get a CT. And its the doctors fault that the patient is fat? Too wide for the scanner? Any responsibility on the patient for being so unhealthy? Any responsibility for being sedentary leading to a PE?
I’m sorry but sure the doc can do better here but at some point human beings need to have some accountability for their own health.
Great post by the way.
1) LISTEN TO THE PATIENT, HE IS TELLING YOU THE DIAGNOSIS: “I am SOB and have normal chest films” is PE until proven otherwise. This means that you MUST continue to pursue PE, even if it means transfer to another hospital.
2) CLUES TO BADNESS CAN BE FOUND IN THE VITAL SIGNS: The patient’s three very abnormal vital signs makes PE even more likely. Bronchitis does NOT cause SOB and fever and tachycardia and tachypnea. The vital signs alone meet SIRS criteria.
This doctor’s management and discharge disposition clearly rises to the level of negligence.