The ED doctor’s note will be the focus of this documentation review. One important thing to remember about good documentation is that it does not prevent a lawsuit. By the time an attorney even has a chance to read the documentation, the litigation process is already well on its way.
However, good documentation can significantly help your defense once a lawsuit has been initiated.
No matter what the doctor wrote, the plaintiff’s attorney was going to find something to criticize. If the erroneous mentions of chest pain had been wiped from the chart, the plaintiff’s narrative would have merely shifted to another focal point. The internal discrepancies about the patient’s chest pain (or lack thereof) simply made the plaintiff’s job easy.
To help write excellent notes while you are working, use the Documentation Template.
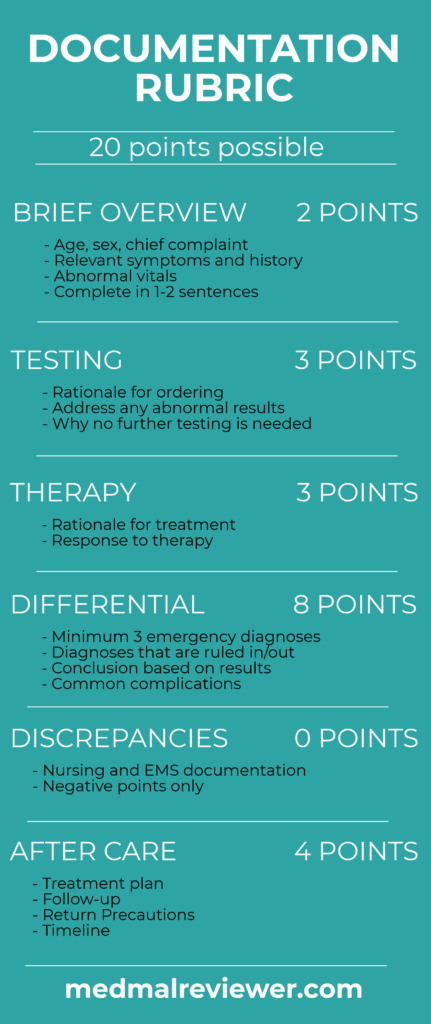
To grade a note that has already been written, use the Documentation Rubric. It focuses solely on the Medical Decision-Making (MDM) of the note.
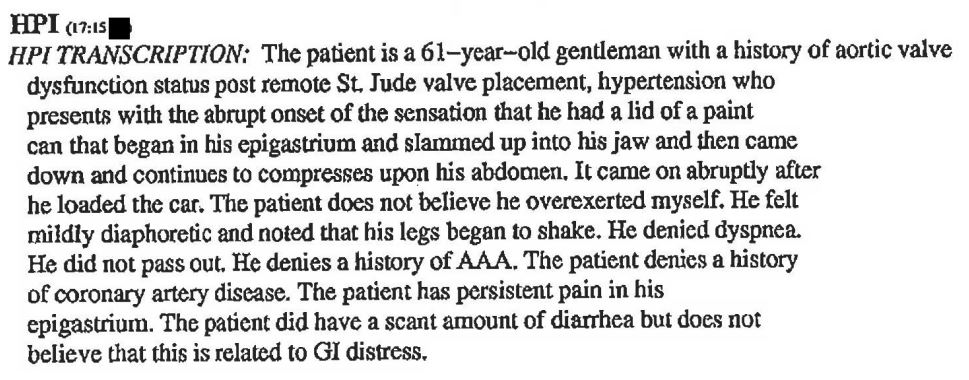
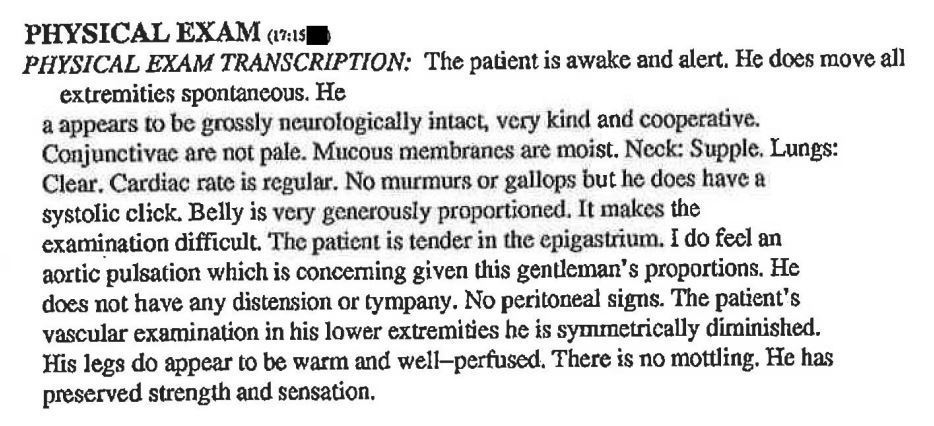
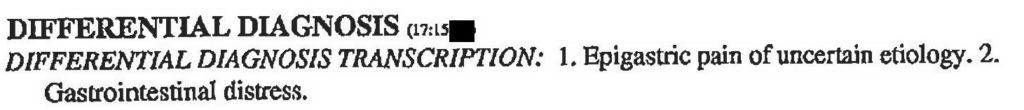
Relevant selections from the note are shown again here for easy reference.
This note scored 13.5/20 points.
Brief Overview: 1.5/2 points
There are many ways to write effective notes. This doctor did not explicitly include a Brief Overview in his MDM, but he does have a well-documented HPI with a good description of the patient’s presentation. It is certainly better than some HPIs which consist of useless click-button statements. In fact, multiple board-certified ER doctors who reviewed this case immediately identified the diagnosis based on reading the HPI alone.
Here is an example of a good Brief Overview that is only two sentences long: “This is a 61-year-old man presenting with sudden onset of epigastric pain that radiates up into his jaw, diaphoresis, shaking legs, and diarrhea. He has a history of aortic valve replacement and hypertension, but his vitals are normal now.”
Testing: 3/3 points
The doctor clearly connects the differential to the tests he is ordering. His orders are rationale based on his concerns. He considered an abdominal aortic aneurysm, so he ordered a CT abd/pelvis. He was worried about acute coronary syndrome so he ordered an EKG and labs including a troponin. He was worried about renal colic, and renal stones would be identified on the CT scan. He even explicitly addresses the fact that the CT abd/pelvis was done without contrast.
The results are then described after the tests are completed. Rather than copy/pasting the results, he describes the few relevant findings. This is the ideal way to document understanding of the results and how they affect the doctor’s mental model of the patient’s presentation. Don’t copy/paste test results.
Therapy: 3/3 points
Zofran and morphine were ordered. These are all perfectly reasonable tests to order. The vast majority of board-certified doctors understand why they were given. Zofran was used to treat his nausea. Morphine to treat his pain. Because these tests are well within normal practice and easily understood, the doctor gets full points even though no documentation is present. Common sense does not need an explanation.
Differential: 6/8 points
This note has a good differential. It is clearly labeled. He considered epigastric pain of uncertain etiology, gastrointestinal distress, abdominal aortic aneurysm, renal colic, acute coronary syndrome. He adds the wastebasket phrase that “these and other diagnoses were considered”.
It is clear that he also considered an aortic pathology, both aneurysm and dissection. In his commentary about the CT results, he states that neither aneurysm nor dissection were visualized. His exam and note strongly demonstrate his concern for aneurysm in his abdomen.
Unfortunately, the failure in the differential was the fact that he did not consider a different anatomical location of the aortic pathology.
This is an example of good documentation of a differential that is missing some key points. It describes his reasoning very explicitly. While the differential does not contain the ultimate fatal diagnosis, the documentation of the differential is excellent.
Discrepancies: -4 points
This is the first MedMalReviewer Documentation Review in which the physician scores negative points. The Rubric only gives negative points to discrepancies, it does not award points for a lack of discrepancies.
There was not just one simple discrepancy. There were multiple contradictions: within the physician’s note, within the nurse’s note, and between the physician’s note and the nurse’s note. It is hard to justify the claim that he had no chest pain when the triage nurse’s documented chief complaint was chest pain, and the doctor’s final diagnosis was chest pain.
The physician documented that he reviewed the nurse’s chart,but does not comment on the fact that the nurse listed chest pain as the chief complaint. This is a missed opportunity.
While it is easy to understand how this happens, it is also easy to understand the legal problem it creates.
Internal consistency within your own documentation is critical, and addressing any discrepancies between the physician and nursing notes is also key.
Aftercare: 4 points
There is a clear plan documented for the patient’s care after the ED. The patient is obviously being admitted. The doctor documented that he had an extensive conversation with the hospitalist.
Overall this is a good note with the exception of the internal and external discrepancies about the patient’s chest pain. It is a stark reminder of the importance of addressing these issues. Ideally, the nurse and doctor can discuss the situation during the patient’s visit or shortly thereafter, and resolve the disagreement. Otherwise, it is a wise idea to politely note the differences and the reasons they exist.
Make your defense attorney’s job easier; write good notes and avoid discrepancies.
Take-home points:
– Thunderclap onset of pain affecting the patient’s trunk: Think Aorta.
– When imaging an aorta or spinal cord, give serious consideration to scanning the entire length.
– Consider other imaging modalities if contrast CT cannot be obtained.
– Make sure your chart is internally consistent and review for discrepancies with nurse documentation.