This case is a doctor’s worst nightmare. The patient had an extremely rare but life threatening condition, which presented with unusual symptoms. It is especially haunting because he spent multiple hours in the ED and hospital, precious time that potentially could have been used to address his aortic pathology.

The difficulty of catching this type of disease is hard to overstate. It was an atypical presentation of a very rare disease. Medical schools teach students the common presentations of most diseases, an approach that is useful for the majority of patients. In residency, most young physicians are fortunate to see the common presentations of rare diseases. However, the atypical presentations of rare diseases (as in this case) represent the once-in-a-career situation that can haunt a doctor and patient for years.
More than one veteran ED physician has suggested that when it comes to emergency aortic pathology, the standard of care may be to miss it the first time. Making the diagnosis is often a matter of luck. Anyone who acts incredulous that aortic pathology gets missed is either blinded by hindsight bias, a plaintiff’s attorney, or has no experience practicing modern Emergency Medicine.
Aortic What?
One critical learning point from reviewing this case is understanding the difference between different kinds of aortic pathology. The terminology can be slightly confusing.
For our purposes, there are 3 basic issues:
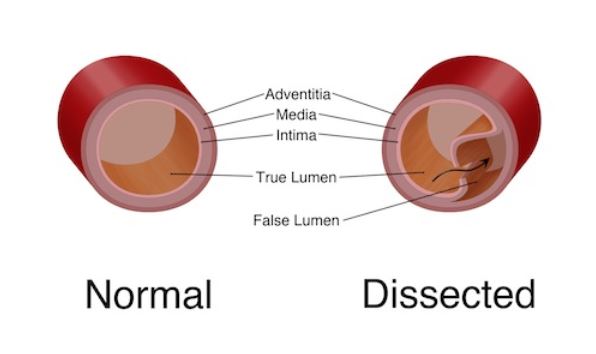
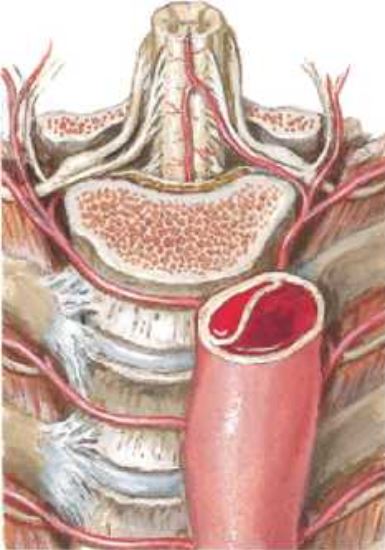
1) Aortic Dissection. A tear along the inner lining of the aortic creates a false lumen. It may initially start as a hematoma in the wall of the aorta and progress from there. It can extend all the way to the aortic valve and coronary arteries, along the length of the aorta and into the iliacs. Pericardial tamponade may occur, along with multiple other complications.
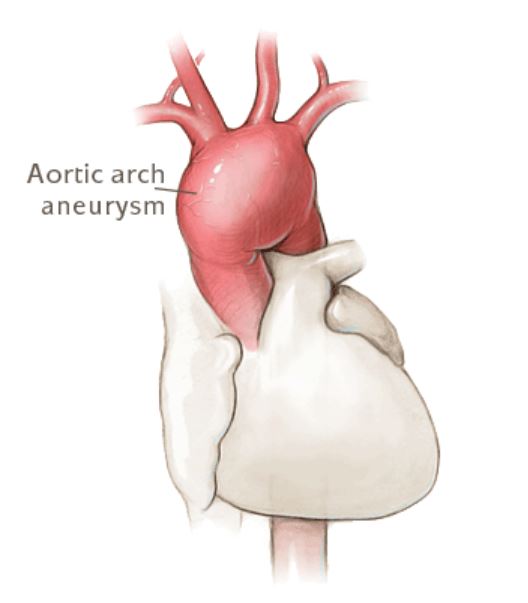
2) Aortic Aneurysm. The lumen of the aorta becomes progressively larger, swelling like a balloon until it eventually ruptures. The swelling of the aorta usually occurs over the course of years, and does not become an emergency until it ruptures. The most common location is the in the abdomen, where it is referred to as an abdominal aortic aneurysm (AAA or “Triple A”). But simply having an aneurysm does not mean the patient has an emergency; there are multitudes of people walking around as outpatients with aneurysms. Its only when it ruptures that it becomes an emergency.
3) Aortic Transection. This is usually referring to a trauma patient. It can occur as a result of penetrating (stabbing, shooting, etc…) or blunt trauma (falls from height, car accidents, etc…). Seeing an aortic transection from trauma is relatively rare given that most patients will rapidly exsanguinate and die before making it to the ED.
These distinctions are important to make, because aortic dissections and ruptured aortic aneurysms are easily confused. For some reason, many students graduate without a clear understanding that an aortic dissection and an aortic aneurysm are two completely different disease processes.
Admittedly, there can be some overlap. A chronic dissection that is mild may eventually lead to an aneurysm. An aneurysm is more likely to have a dissection. However, in the ED, the patient is usually dying of one or the other. It is better to understand them as separate entities and know they can overlap, rather than to refer to every aorta problem as a “dissecting aneurysm”, which is often an inaccurate description.
Anatomic Location
The aorta travels through both the chest and the abdomen. The aorta can suffer one of these critical issues at EITHER of these anatomical segments.
An aortic aneurysm can occur in the chest or the abdomen.
A aortic dissection can occur in the chest or the abdomen.
This was probably the key failure on the part of the ED doctor. He considered aortic pathology. In fact, it was very high on his differential. Unfortunately, the patient’s presentation did not guide him to the correct anatomical location.
A dissection is most commonly divided into two types. Type A is any dissection that is affecting the ascending aorta, up to the left subclavian artery. Type B is any dissection that is not affecting the ascending aorta.
It is easy to focus only on abdominal aortic aneurysms and forget about those in the chest. Granted, most aneurysms are in the abdomen. And saying “Triple A” rolls off the tongue nicely. But don’t forget about both chest and abdominal aortic pathology.
Final Diagnosis
In this case, the final diagnosis is not entirely clear. No autopsy was conducted, so the information we have is from the interventional cardiologist. He felt that there was a thoracic aortic aneurysm with fistula to the pericardium.
This would be an unusual presentation of a thoracic aortic aneurysm. There are certainly case reports of thoracic aortas resulting in fistulas, but the fistula usually forms to the airway. There are also reports of fistulas forming from the aorta to the pericardium but most are related to infection (here and here).
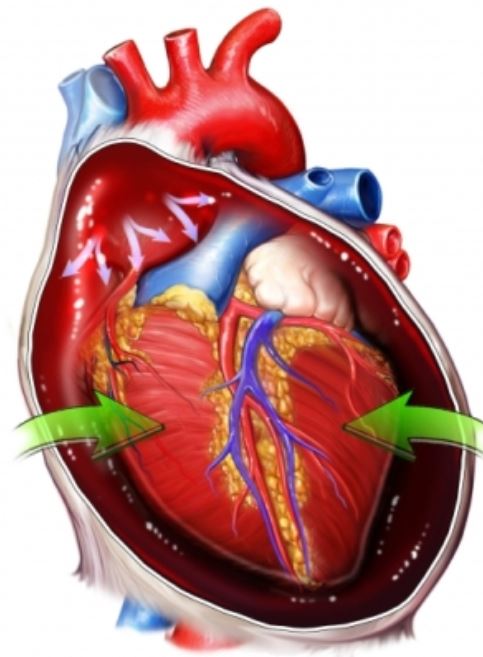
If this patient truly did have an anuerysm with fistula to the pericardium, it was a rare complication of an unusual presentation of a rare disease. A more common cause of emergency aortic pathology associated with pericardial effusion would be an aortic dissection. The report from the cardiologist is the best information we have, but any informed reader will question the final diagnosis. An autopsy would have provided more definitive information.
Chest pain
The patient’s lack of chest pain was the unfortunate truth that probably had the biggest impact on the bad outcome. Based on the documentation, workups, and depositions of all 3 doctors, it seems fairly clear that he never had chest pain. If only one person had documented no chest pain, it would be easier to suggest a miscommunication, but he denied it to multiple reliable healthcare workers. The consistency of this story is striking.
Granted, the chief complaint was listed as chest pain. This is easily explained by the fact that chief complaint is often a rapid and sometimes inaccurate description of the patient’s true presentation. It was simply the easiest chief complaint to record to get the patient back into an ED room quickly. As every physician knows, the chief complaint is often inaccurate or doesn’t tell the entire story.

The final diagnosis of “chest pain” is easy to understand as well. The patient needed to be admitted on telemetry, and the physician knew the easiest way to justify telemetry was to list the final diagnosis as chest pain. The final diagnosis in this case was not a true final diagnosis, it was simply a means to an end.
Typical symptoms
The description of the patient’s pain is very atypical. The pain that slammed up from his abdomen into his jaw, with legs vibrating, is oddly specific. This description of pain is unusual, and raises some red flags for dissection (albeit with the benefit of hindsight). Patients do not usually describe their discomfort using these comparisons and adjectives.
He did not have the classic description of pain radiating to the back. In fact, the history in patients with aortic dissection is notoriously varied. Many do not have the classic description of pain. The exam is often reliable; classically taught findings such as unequal blood pressures in the bilateral arms may not be present.
Thunderclap, Radiating, Trunk Pain
There are several attributes of a history that should raise a flag for aortic dissection. They are reviewed in this excellent blog post and podcast from RCEM. Pain is the most common presentation, but bear in mind that some patients present with no pain.
One key feature of the pain is that it may be sudden onset. Just like the mental association between thunderclap headache and subarachnoid hemorrhage, building a mental model connecting thunderclap trunk pain and aortic dissection may be beneficial. The pain is most often sharp or tearing. Radiation of the pain or other unusual symptoms (such as legs vibrating) to other body areas can guide the astute physician to the diagnosis as well. The abdomen is the third most common site of pain, following the chest and back.
Imaging
If the patient actually had chest pain, a chest x-ray would likely have been ordered. The plaintiff’s attorney’s argument centered around the logical connection between chest pain (even if inaccurately documented), and a chest x-ray. However, there is even some discussion among academic ED doctors about which chest pain patients need an x-ray. A study suggested that chest pain patients with no history of CHF, no history of smoking, and no abnormalities on lung auscultation can forgo chest x-ray. Their study had 529 patients and the rule was 100% sensitive. While there may be some academic discussion around the need for chest x-rays, by far the consensus in EM will be that all chest pain patients require a chest x-ray.
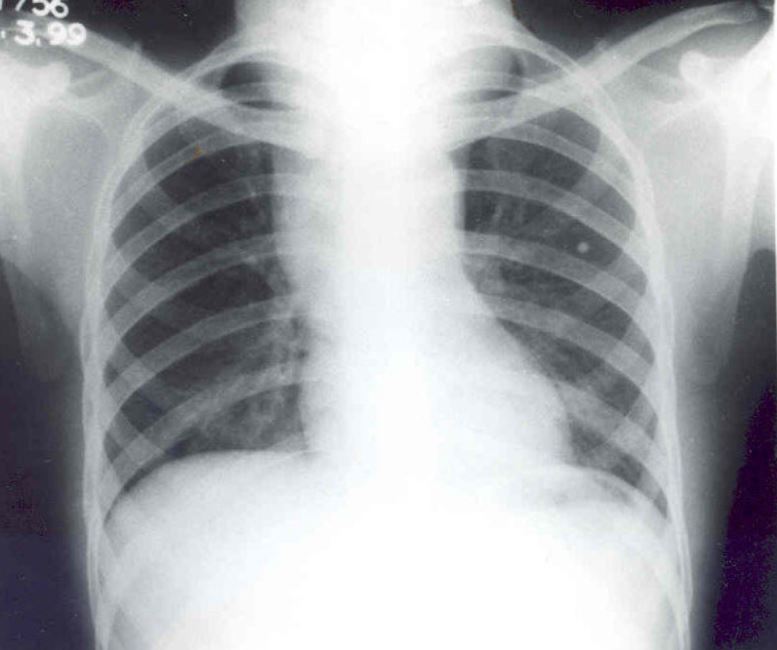
Whether the patient had an aortic aneurysm or aortic dissection, a contrast CT study of their chest would have provided clarity. The patient did report an allergy to contrast dye, complicating the situation. During the wife’s deposition, she could not remember what his reaction was, as she was not in the room when it happened. Given the lack of any clear memory, there is some degree of doubt that it was actually an anaphylactic reaction. Asking the patient about the type of contrast reaction may have been useful. While there are some patients who should never receive contrast, some patients can be treated with Benadryl and steroids and still go ahead with the scan. This is especially important when a patient may have a life-threatening disease and it is the only obstacle in the way of obtaining the gold standard test.
Another imaging option would have been an ultrasound. An ED doctor with an ultrasound on this patient’s chest may (or may not) have identified an issue at the aortic root. An aneurysm or dissection could theoretically be identified, although it can’t be completely ruled out if negative. A pericardial effusion could also have been identified.
An echocadiogram could be ordered if the physician was trained prior to widespread adoption of ultrasound. However, this is not available in many EDs. Even in large medical centers, may not be completed until the next day. Unfortunately, obtaining a stat echo is from the ED is extremely unusual, let alone a stat unscheduled TEE with only marginal suspicion for the disease.
MRI was another option for this patient. It is unclear if the patient would have been eligible for an MRI or if the ED had one. But it is worth considering in the right patient.
Aortas and Spinal Cords
This case provides an opportunity to review a recurring issue when ordering imaging. When a physician is concerned for serious aortic pathology, or serious spinal cord pathology, give very careful though to imaging the ENTIRE length of the aorta or spinal cord. In Case 5, the physician ordered an MRI of the lumbar spine, and missed the critical diagnosis at the thoracic spine.
The history and physical exam are often helpful for locating what part of the body needs imaging. Unfortunately, the history may not be completely reliable, especially when it comes to the aorta and spinal cord. It is tough to review cases in which the physician ordered the right test, but just barely missed the diagnosis because the wrong area was imaged. The importance of imaging the entire aorta or spinal cord is not based on a peer-reviewed study, but it is certainly a recurring theme that has been associated with tragic patient outcomes and lawsuits.