The operation was scheduled at an outpatient surgical center. The neurosurgeon and orthopedic spine surgeon were partners at the facility.
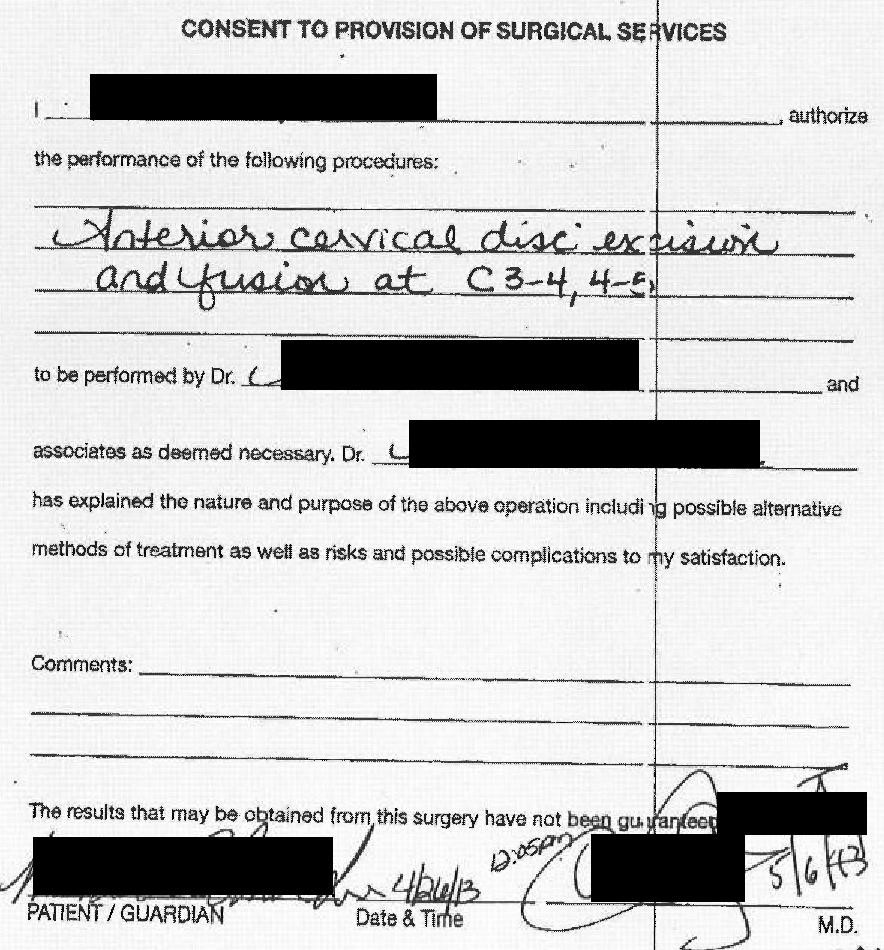
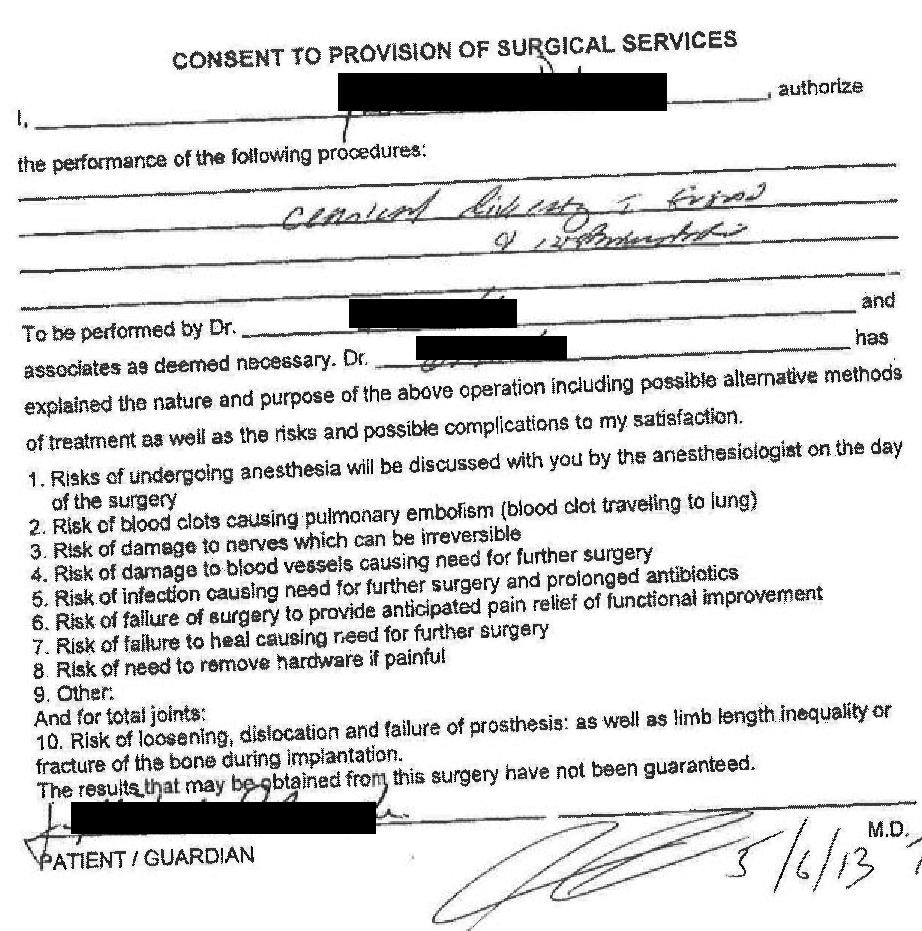
The patient checked in the morning of the operation. He met the anesthesiologist and signed consent forms from both of the surgeons.
The patient was brought back to the operating room. He was intubated safely and the operation began. The neurosurgeon operated first and performed the initial dissection. The orthopedic spine surgeon was in the building but was waiting outside the OR for his role in the operation.
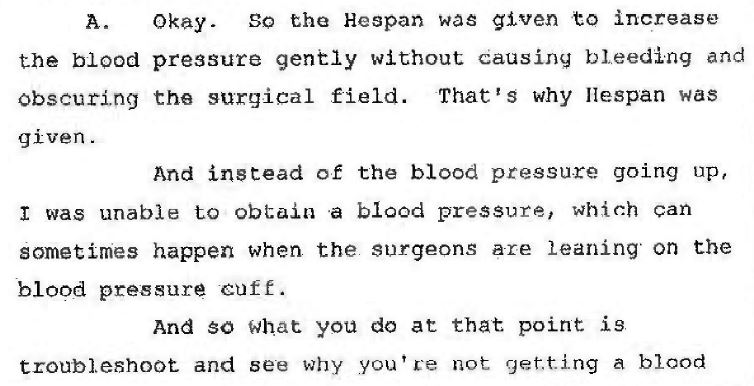
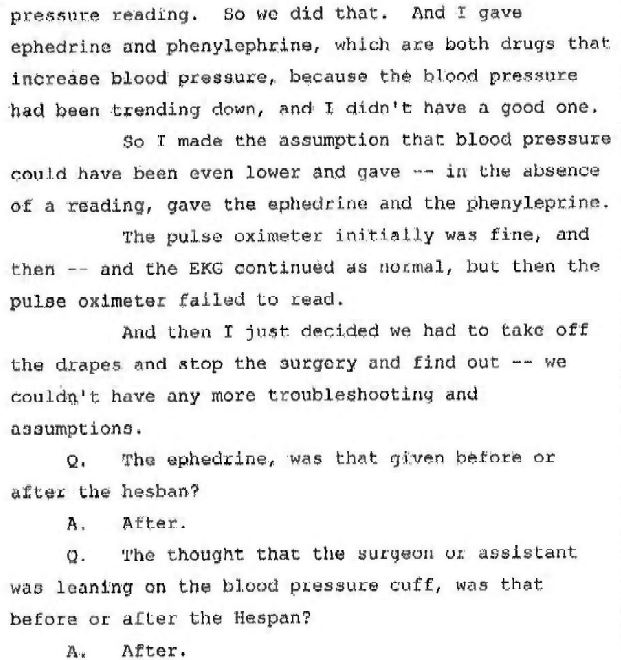
While the neurosurgeon was performing the initial part of the surgery, the patient’s blood pressure drifted downward slightly. The anesthesiologist started troubleshooting the blood pressure. She had Hespan (a colloidal volume expander) in a cabinet in the OR. She reached into the cabinet and gave a bag of fluids, but the blood pressure continued to drift down. She thought the surgeon may be leaning on the blood pressure cuff, giving a false reading. She gave medications to increase the blood pressure.
The anesthesiogist would later be questioned about her actions in a deposition. Her explanation is shown here:
She continued trying to troubleshoot the low blood pressure. Her documentation of the next events are shown here, only for Med Mal Reviewer subscribers.
The patient had decompensated over the course of several minutes, and had complete cardiovascular collapse. The code continued in the OR as the anesthesiologist and nurses fought to save his life.
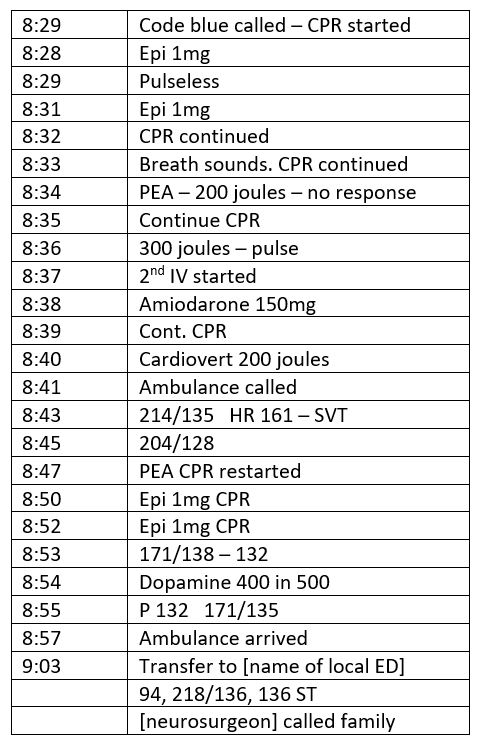
The patient had a pulse when he was loaded onto the ambulance and taken to the nearest ED. To see the EMS and ED records, continue to the next page.