The Documentation Rubric applies to any undifferentiated patient in the acute care setting.
We will address Dr. B’s documentation here.
Note that Dr. R did not write anything in the patient’s chart. This is extremely bad form. If you see a patient or make recommendations on their care, you must write a note.
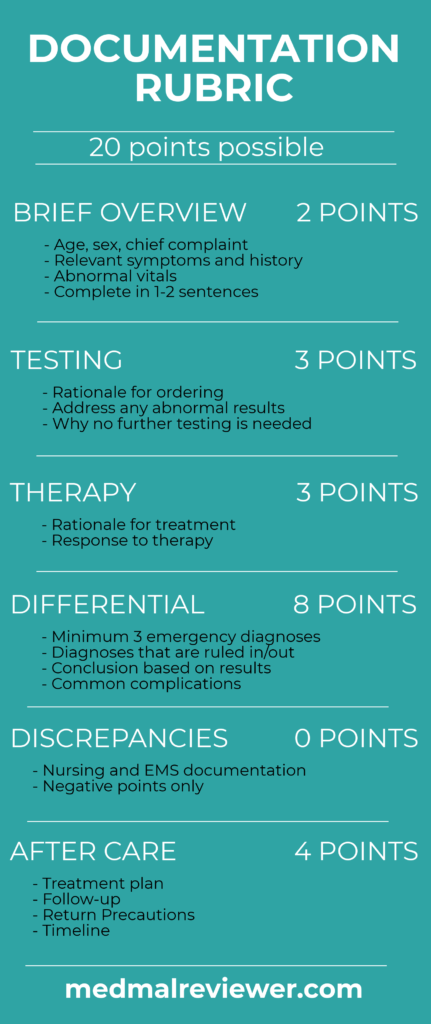
This note scored 12/20 points.
Brief Overview: 2/2
Dr. B adequately describes the presentation of the patient, emphasizing that he was in extremis on arrival. He includes abnormal vitals and initial interventions that were performed, including intubation and IV fluids. His physical exam denotes the abnormalities identified.
Testing: 2/2
The physician documents his discussion with the surgeon regarding what imaging should be ordered. He later reviews the lab results as well as the pertinent imaging findings. As highlighted in other cases, they did not simply copy the imaging results, but presents an overview of the imaging as it pertains to the ultimate disposition, commenting specifically on the lack of intracranial blood and intra-abdominal bleeding, the presence of c-spine fractures and a femur fracture with bleeding. The emergency physician details his discussion with the orthopedic surgeon and their recommendation.
Therapy: 1/3
The emergency physician uses one brief comment (“The patient maintained a decent blood pressure on Levophed between the 80 and 116 systolic…”) to summarize the several hour span that the patient was in the emergency department. Detail is lacking regarding response to specific doses.
The “failure to provide prompt blood products” to the patient was a keystone of the complaint by the plaintiff. Unfortunately, the administration of blood products was not mentioned at all in the original MDM, only appearing in the addendum added afterward.
This would be a useful place to document that FFP and platelets are not available at your center. As mentioned previously, you could additionally document if you verbally asked for medications or blood products before the computer order made it into the chart. Critical care cases are often the only time where verbal overrides of orders are allowed in the emergency department, and there may not be real-time nursing documentation to record this.
Differential: 5/8
The differential of a trauma patient is not very broad compared to medically ill patients, however the differential becomes the crux of the defenses’ argument. The physician notes a few diagnoses that would determine whether transfer would be warranted, including intracranial hemorrhage or intra-abdominal bleeding. Later on in the end of the note, they detail four diagnoses in their clinical impression. A clinical impression is not the equivalent of a differential diagnosis, but rather is the narrowed down differential after the workup. However, if they were indeed using the vasopressors to treat neurogenic shock, this is where they should have mentioned it. If vasopressors were only used as a temporizing measure for hypovolemic shock due to the delay of blood at a community center, that could have also been mentioned that reasoning earlier in their MDM.
Discrepancies: 0/0
There were no clinically significant differences between the physician’s note and the RN or EMS documentation.
After Care: 2/4
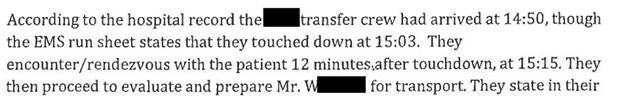
There is a lapse in documentation between the arrival of the flight crew at 15:03 and the patient coding at 15:57. According to a deposition of a member of the flight crew, Dr. B was not called back into the room until the code was called, and was unaware that the patient and flight crew hadn’t left yet.
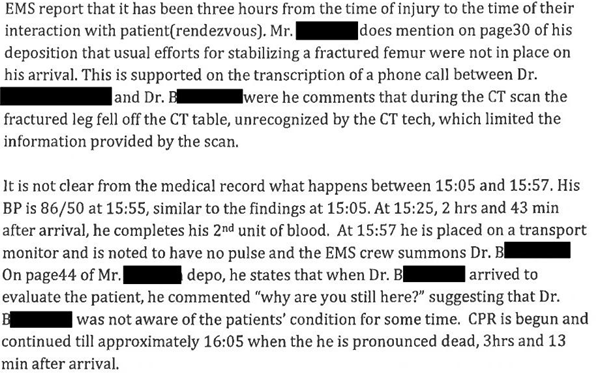
This delay often occurs when transportation arrives — the referring team breathes a huge sigh of relief and walks away to take care of the rest of the emergency department full of patients. According to EMTALA, the referring physician is responsible for the patient until the patient arrives at the receiving facility.6 If Dr. B had been aware that the patient was still in his emergency department, he may have been able to order additional resuscitation (e.g. transfusion of the other 2 crossmatched units of blood products) or other interventions prior to the patient coding.
Take Home Points
– Hemorrhagic shock should be treated with urgent blood transfusion.
– Norepinephrine is not an acceptable treatment for hemorrhagic shock
– Critically ill trauma patients should be rapidly transferred to a trauma center
– Time moves fast in the trauma bay. What feels like 5 minutes may actually have been an hour. Move smoothly but quickly.
– A physician who sees a patient must document a note
You can’t find cases like this anywhere else. Join the email list now to get them delivered to your inbox!