This case involves 2 different physician notes, and both will be evaluated. The Documentation Rubric will be used to assess both notes in the same standardized way. As we will see, one of the notes provides an excellent example of good documentation, but the second note is nearly useless.
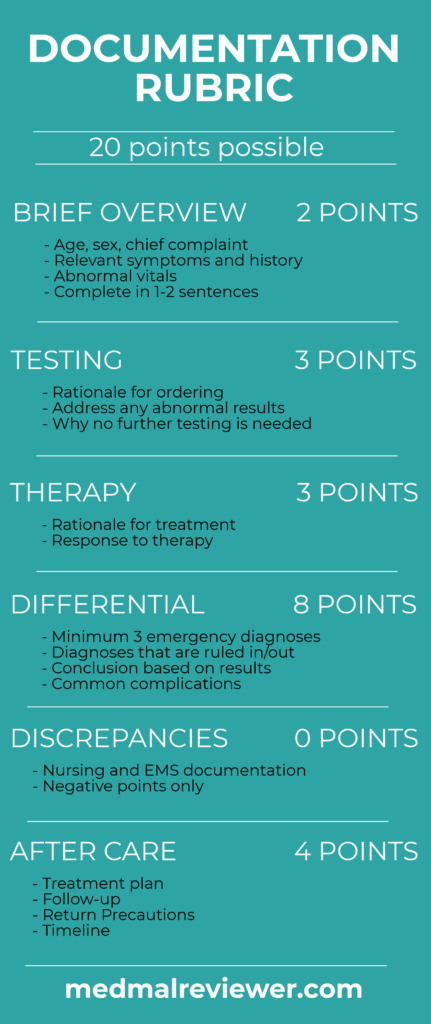
The Documentation Template was created for clinicians to use while working, in order to create defensible documentation. This is specifically focused on the medical decision-making (MDM) portion of the note, not the history, social/family history, past medical history, exam or ROS. The Documentation Rubric was created for grading MDM sections.
The first physician used both a T-sheet and an additional dictation to describe his assessment and care of this patient. As seen in previous cases, T-sheets allow for rapid documentation that is focused on billing. However, they are also very brief and often times do not not facilitate an effective defense if a physician’s care is questioned. This doctor was wise to create additional documentation to defend himself. His note earned a score of 17/20.
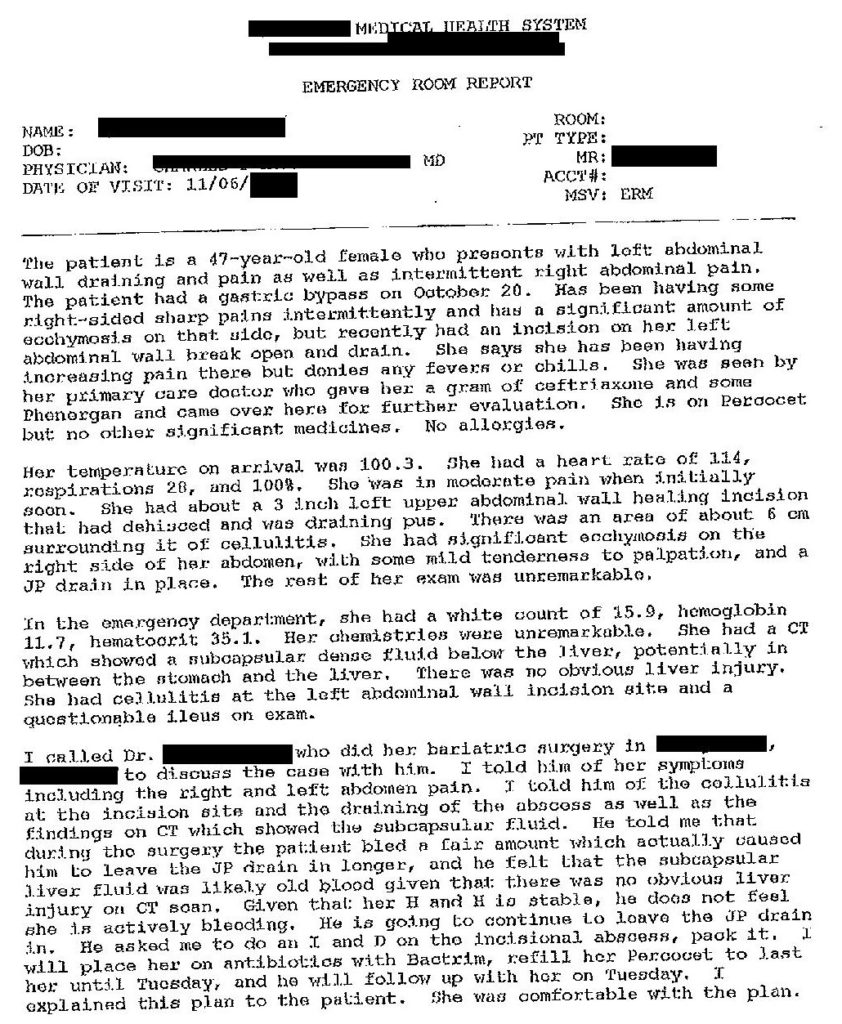
Brief Overview: 2/2
There is an effective brief overview. If anything, it may actually be somewhat excessive. The entire first paragraph of his dictation concerns her presentation to the ED. It is an effective distillation of her presentation to the ED. He also rehashes her vital signs, indicating to the reader that he has reviewed them and taken their significance into account.
Testing: 2/2
The tests that he ordered are reviewed. The labs and imaging he orders are logical and easily understood by an EM physician. He reviews the relevant results on both the labs and the CT. Rather than simply copy/pasting results (a terrible practice that does not indicate comprehension and just wastes space), he indicates his comprehension of the results and synthesis into his care of the patient.
Therapy: 2/3
One area of improvement in this documentation would be to discuss her therapy, and her response to her ED treatment. He initially mentions the medications she received prior to ED arrival and what she had been prescribed as an outpatient. There is little discussion of her response to therapy, although we know from nursing documentation that her pain started at a 9/10, improved to 4/10, then got worse back to a 9/10. An assessment of this change and the improvement in her vitals would have been worthwhile.
Differential: 6/8
While the physician never mentions an explicit differential, various items are mentioned throughout his dictation. He mentions cellulitis, possible abscess, ileus, liver injury, and also discusses the potential for bleeding in her abdomen. One particularly encouraging aspect of his assessment, is that he mentioned findings that were ruled out (liver injury), as well as things that have been ruled in (cellulitis and abscess). A differential can be more than a list of diseases the patient might have, it can also include a few items that have been ruled out, whether that is based on history, exam, or testing.
Discrepancies: None
Aftercare: 4/4
The aftercare discussed in this note is excellent. The physician clearly lays out a plan to treat her with Bactrim and Percocet, which will last her until a follow-up appointment on a specific day. The time frame is well-delineated. He gave her return precautions for general issues (“if symptoms worsen”) as well as specific guidance (“particularly if she gets a fever or has increased pain”). He goes even further, and states that he discussed these things with the patient directly, that she understands them, and is comfortable with the plan. These aftercare instructions are documented extremely well. They allowed the healthcare team another opportunity to save the patient’s life, a chance that was unfortunately squandered.
Another item to cover is the documentation of the conversation with the consultant. He states what information was communicated to the consultant, what they discussed, and the recommendations that were made. He even includes the consultant’s rationale for his recommendations.
Overall, the first physician’s note was superb. It provided a clear explanation of his thinking and the care rendered to the patient. It set him up for an effective defense by his legal team. Even though future events resulted in a lawsuit, the doctor can rest easily knowing that he provided good care and documented it in a thorough and careful fashion.

The note from the 2nd doctor was unfortunately a disaster. It is brief and provides little insight into his thinking. It is very confusing to review the record and try to understand why he sent the patient home without any further testing. Even the EMS crew wrote more than him. His note provides no rationale for the bizarre and dangerous decision to discharge her home. This note scored 2.5/20 points.
There is no brief overview aside from a history that consists of a few words (0.5/2 points).
No testing was ordered, and worse, there was no explanation for why he did not order any testing (0/2 points).
Some of the medications he ordered were logical (pain medication, antibiotics, antiemetics), but there was no explanation of her response to these medications (1/3 points).
No differential was recorded, there was no sign he even thought about what could be causing her return to the ED. This is the most problematic issue, it appears he did not even stop to consider that her condition had developed into an emergency or what could be causing her symptoms (0/8 points).
The aftercare does show a plan (to fill her scripts). However, he makes several odd recommendations. She was told to be NPO for 24 hours (odd considering her elevated heart rate), and to have “small pieces toast!” (1/4 points).
Good documentation helps EM physicians provide good medical care. It allows for a moment of reflection on the rationale for the care given each patient. There is almost nothing that the 2nd physician could have documented to defend his care, but writing a more thorough note may have helped him realize the shortcomings of his plan in real time.
The few extra seconds required to write good notes can help provide a moment of reflection to avoid outcomes like this, and will help defend your care if it is ever questioned.