For this case we will review the first physician’s documentation. His documentation will be reviewed in the standard format, using the Documentation Rubric. His note is a fairly standard EM note.
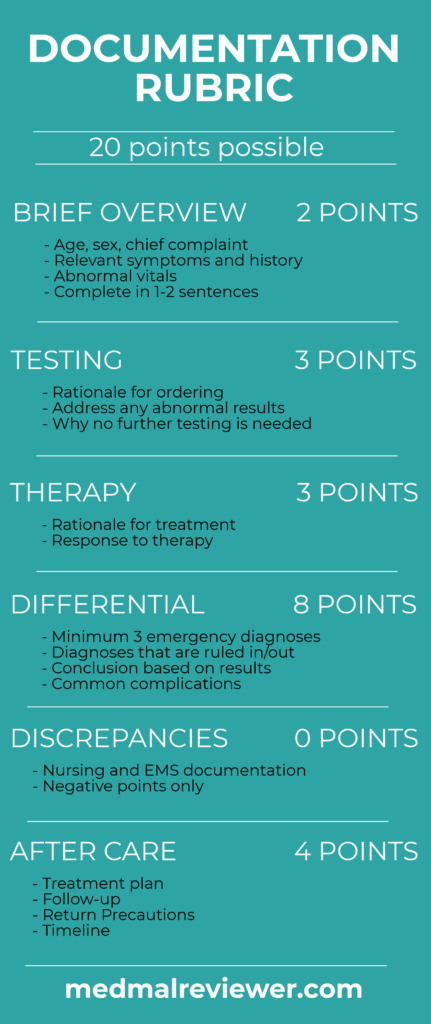
The Documentation Template was created for clinicians to use while working, in order to create defensible documentation. This is specifically focused on the medical decision-making (MDM) portion of the note, not the history, social/family history, past medical history, exam or ROS. The Documentation Rubric was created for grading MDM sections.
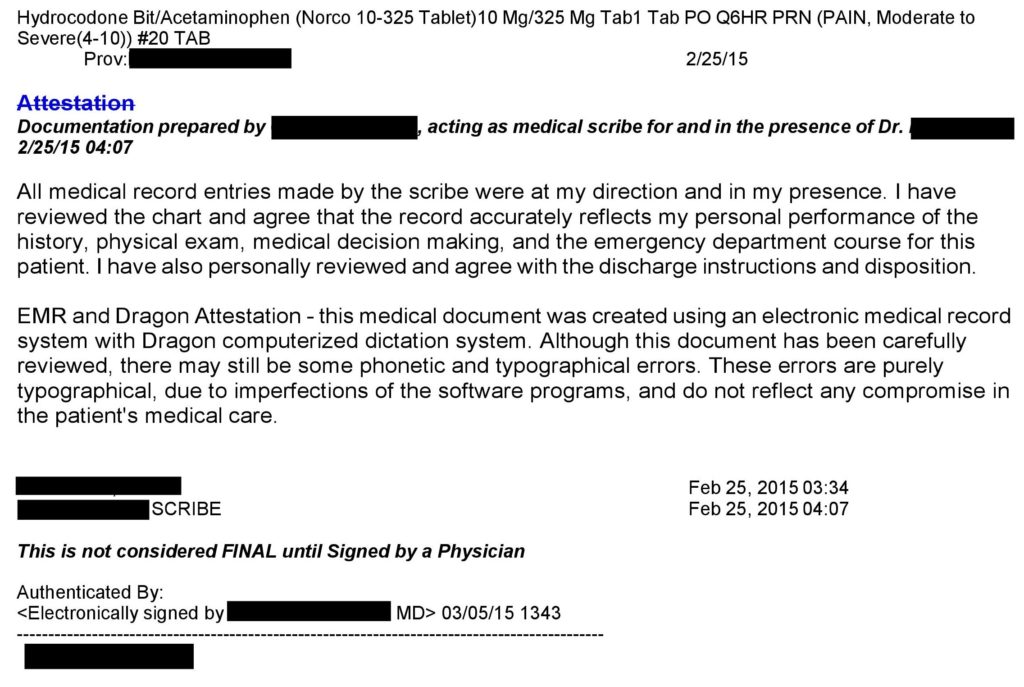
This physician’s note was written in a standard format that is easy to follow and understand. His note ultimately had a score of 10/20.
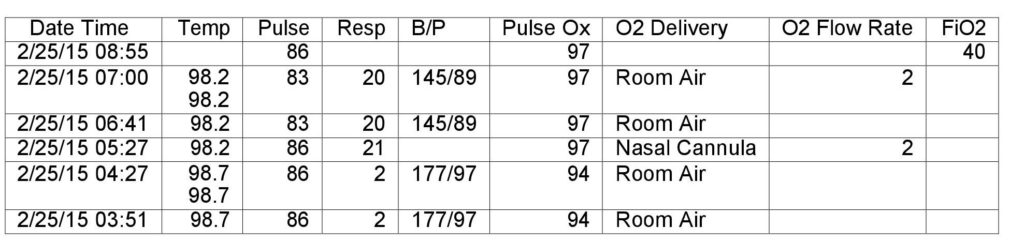
It shown again here for easy reference:
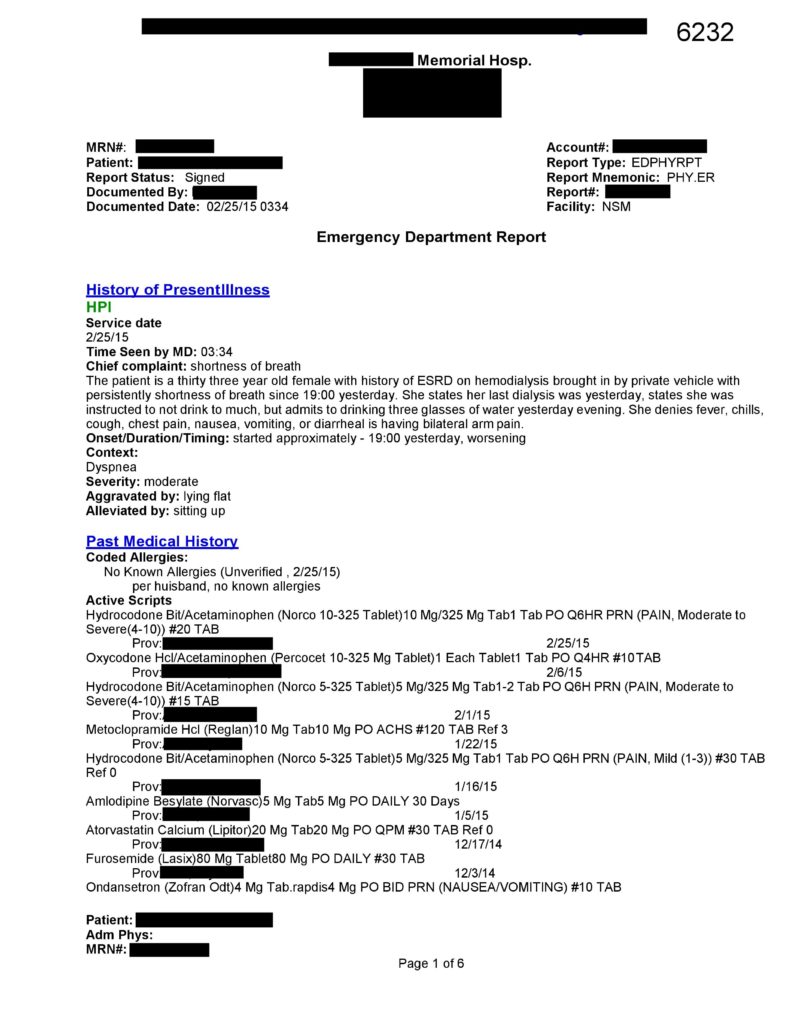
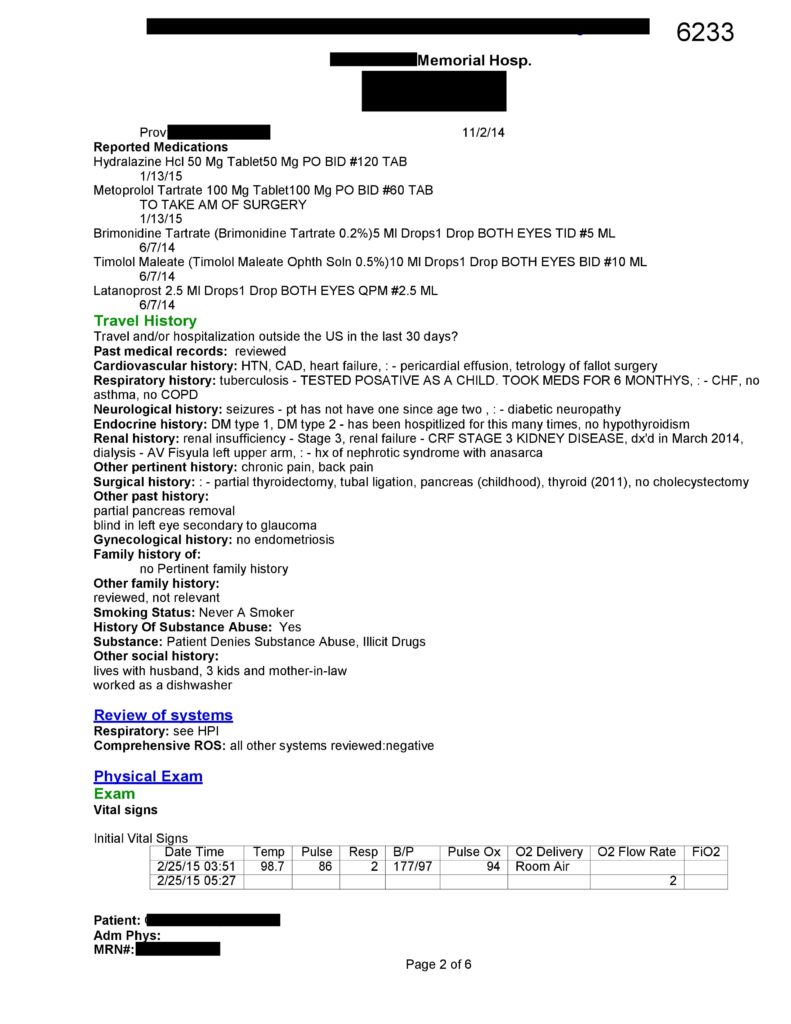
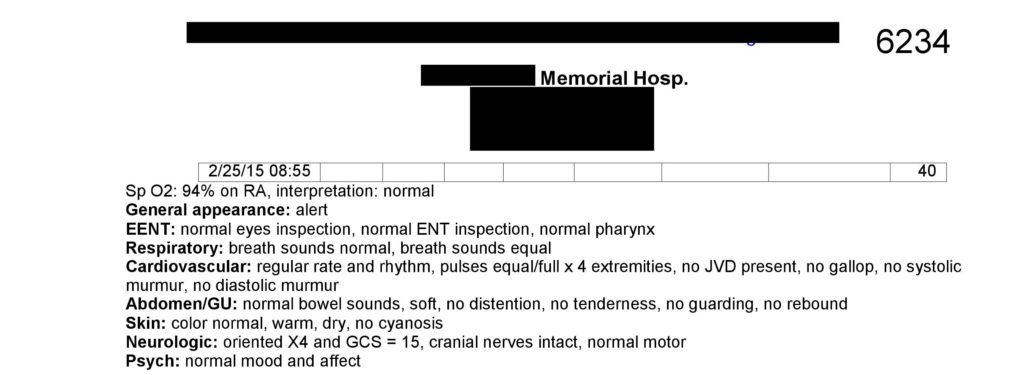
Brief Overview: 1.5/2
An effective brief overview exists at the start of the history of present illness. There are many effective ways to write a good note, but the Documentation Template recommends including an 1-2 sentence overview of the pertinent facts at the start of the Medical Decision-Making portion. This would also include any abnormal vitals.
Testing: 3/3
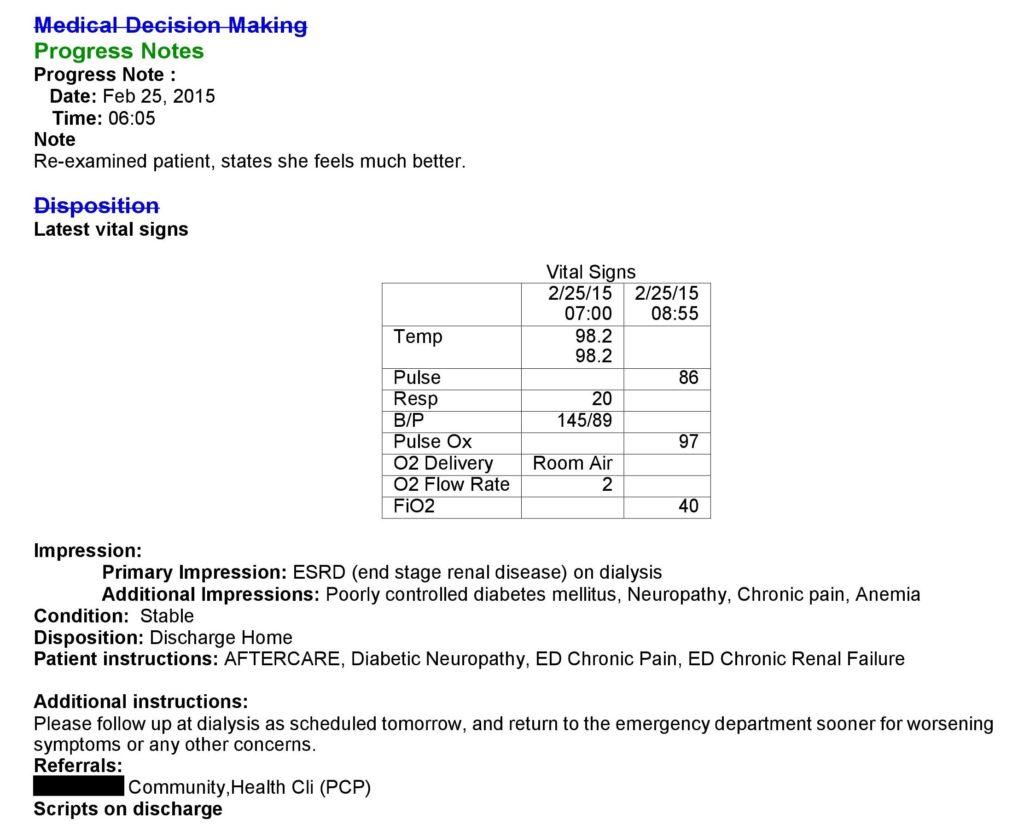
The tests that are ordered are not specifically regurgitated in the note. However, they are all logical tests that can easily be understood from the perspective of an EM physician. This consists of a CBC, CMP, cardiac panel, BNP, chest x-ray, and an EKG. Despite the expert witness claims, the tests are well within the standard of care. No explanation is required if they are clear and logical to an EM board certified physician.
Therapy: 2/3
This is the area that ultimately resulted in significant problems for the patient. The insulin ordered is an appropriate response to her hyperglycemia, and Zofran was obviously given as she was nauseated. Points were deducted as the decision to give Dilaudid seems inappropriate, albeit with the benefit of hindsight. The only mention of pain is a jumbled sentence at the end of the HPI that mentions bilateral arm pain. Even if she had some element of discomfort from neuropathy related to her diabetes, opiates are generally not effective. Documentation of treatments ordered is not necessary if they logically follow from the patient’s complaints, but if there is no logical connection, the physician is wise to explain the rationale behind his orders.
Differential: 2/8
No clear differential is mentioned in this note. There is a list of various diagnoses included in the impression, but no indication of the physician’s prospective differential diagnosis. In a patient with shortness of breath on dialysis, this could include mention of fluid overload, ACS, pneumonia, pneumothorax, among others. It is also important to document a differential via negativa, meaning documentation about what related diseases can be ruled out by H&P alone. In this case it could have included an explanation of why the physician did not think the patient had a pulmonary embolism, pericardial effusion, etc….
Discrepancies: -2
This is one of the major issues with this note. The nurse’s documentation clearly lists a potentially fatal allergic reaction to Dilaudid, but the physician documented that there were no allergies. This is the issue that led to the patient’s bad outcome. Plaintiff’s attorneys are known to dig through records and note any discrepancies, which are easily used to make the healthcare team look incompetent.
Aftercare: 3.5/4
Aftercare has 3 critical elements: plan of care after discharge (prescriptions, etc…), follow-up, and return precautions. These elements all need a specific timeline. The patient was clearly instructed to return if her condition worsened. She was given a prescription for pain medication. She was instructed to follow-up with her primary care office, although a specific timeline would have been helpful.
Conclusion
This note is well within the standard of what most EM physicians would document for this patient. Keep in mind that the Rubric used to grade these notes is used to model a perfect note using only one method of writing notes. Many other reasonable approaches exist. Use of this Med Mal Reviewer Documentation Template is not necessary, but does provide an excellent framework for physicians interested in improving their documentation.
Addendum
The primary issue in the documentation of this case concerns the second physician’s addendum. It is shown below.
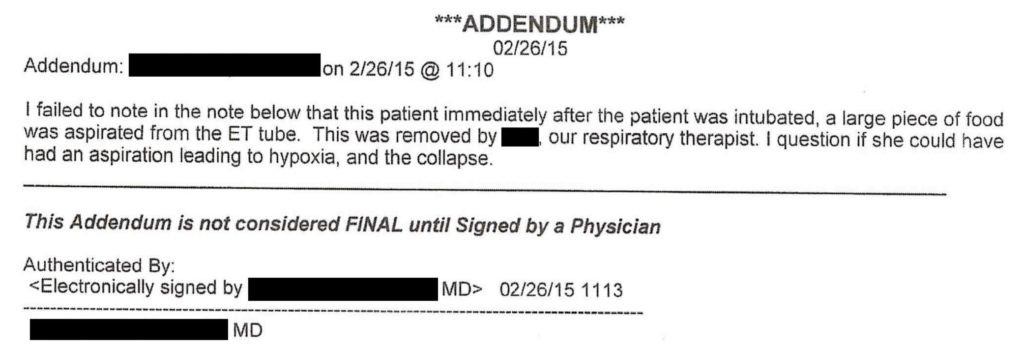
While discussing this addendum, we will refrain from passing judgment about whether it is a true statement or not. Regardless, it is ripe for attack by the plaintiff’s attorney. There is an obvious potential motive behind this, which is to protect the physician’s colleague. Passing the responsibility for the bad outcome to the patient would potentially help the first physician avoid responsibility.
Making addenda to a patient’s chart, especially after a bad outcome is recognized, is a dangerous medico-legal maneuver. While the truth should be accurately documented, physicians in this situation would be wise to consult with their hospital’s legal team before proceeding.
Case 10 Key Points
– Carefully review nurse documentation
– Dilaudid has little benefit for neuropathic pain but significant risks
– Beware multifactorial respiratory depression
– Healthcare leaders should focus on building safe systems
– Avoid adding addenda to a chart after a bad outcome